If you’re living with diabetes, you know that keeping track of your blood sugar is a big part of staying healthy. But you might be wondering:
“Should I keep using my blood glucose meter (fingersticks), or is a continuous glucose monitor (CGM) better for me?”
As a registered dietitian and CDCES, I help people with diabetes understand their options and feel more confident in their choices. Let’s walk through the differences between a blood glucose meter (BGM) and a continuous glucose monitor (CGM) so you can decide what’s best for you.
Option 1: Fingerstick Meter (BGM)
This is the traditional way to check blood sugar. You prick your finger, place a drop of blood on a test strip, and get a number in a few seconds. It gives you a snapshot of your blood sugar at that moment in time.
Pros:
- Affordable and easy to find. Most insurance companies cover BGMs and you can also purchase BGMs and testing strips for a relatively low cost over the counter.
- Good for occasional checks or before/after meals
- Doesn’t require wearing a device
Cons:
- Requires multiple finger pricks a day if you’re checking often
- Doesn’t show how your blood sugar is trending (going up or down)

Option 2: Continuous Glucose Monitor (CGM)
A CGM is a small sensor that’s placed on your belly or arm, which checks your glucose every 1-5 minutes. That’s up to 288 glucose readings in a 24 hour period! Placing the sensor on your skin is easy and relatively painless.
Pros:
- Shows your glucose trends (whether it’s rising, falling, or steady)
- Sends alerts to your phone or reader if your blood sugar is too high or low
- Reduces or eliminates fingersticks (depending on the model)
- Helps connect your food, exercise, stress, and sleep to your numbers
Cons:
- Can sometimes be more expensive (depending on insurance), however, there are now options that can be purchased over the counter without a prescription for a more reasonable cost.
- Slight lag time (measures glucose from fluid under the skin, not from blood)
- Requires wearing a sensor
Why can BGM readings be different from CGM readings?
Blood Glucose Meters (BGMs)
When you use a fingerstick, you’re measuring glucose directly in the blood — specifically in capillaries. This gives you a very immediate and direct picture of your glucose level at that moment in time.
Continuous Glucose Monitors (CGMs)
A CGM sensor has a tiny filament that sits just under your skin and measures interstitial fluid glucose — the fluid that surrounds your body’s cells. Glucose from the blood moves into this fluid or space, so it’s slightly delayed compared to what’s in your bloodstream. This delay is called “lag time,” and can be up to 5 to 15 minutes behind a BGM reading
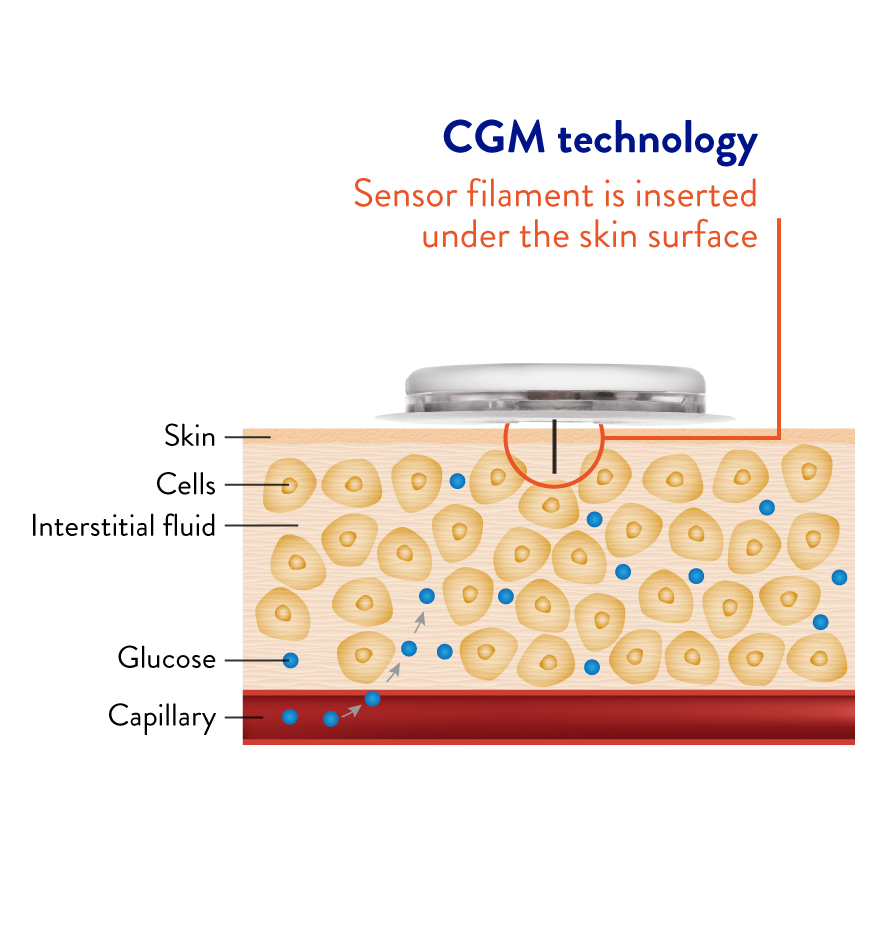
Image source: https://payer.freestyle.abbott/us-en/Resources/what-is-cgm.html
More on Why CGM and BGM Numbers Don’t Always Match
Because CGMs and BGMs are measuring different body fluids, and because of the natural delay in glucose movement from blood into interstitial fluid, their readings often differ — especially when glucose is changing quickly.
Common Situations Where You Might See a Difference
- After eating or taking insulin (glucose levels may be rising or falling fast)
- During exercise
- When correcting a high or treating a low
- If you’re dehydrated (can affect interstitial fluid readings)
- If your CGM sensor is newly inserted or nearing expiration
What to Focus On Instead
Instead of comparing numbers side-by-side, focus on:
- Trends and direction arrows on the CGM
- Whether glucose is steady, rising, or falling
- Time in range (how long your glucose stays between 70–180 mg/dL, or your personal glucose target)
- Confirming symptoms with a fingerstick if needed (e.g., when you feel low but CGM shows normal)

Real-Life Example
Imagine you’re about to go for a walk, with a meter you would check your blood glucose before you go. The reading may be 110 mg/dL, but you won’t know if it’s dropping during your walk. With a CGM, you would see that your number is 110 and dropping, so you could grab a snack before heading out so you don’t experience hypoglycemia.This real-time information can help you feel more confident and avoid surprises and hypoglycemic events.
What I Tell My Clients
Whichever tool you use, you are not just a number. Glucose tools are there to help you learn, not to judge. Some days will be more in range than others — and that’s okay. The goal is progress, not perfection, and to find the tool that works best for you. When you understand your numbers, you can make informed decisions about your food, movement, medications, and more.
If you’re curious about trying a CGM, talk to your healthcare provider or diabetes educator. Many insurance plans now cover them — and they can be a game-changer! You deserve care that’s personal, practical, and empowering.
Written by our Registered Dietitian and board certified specialist, Hayley Perkins, RDN, CDCES.

+ show Comments
- Hide Comments
add a comment